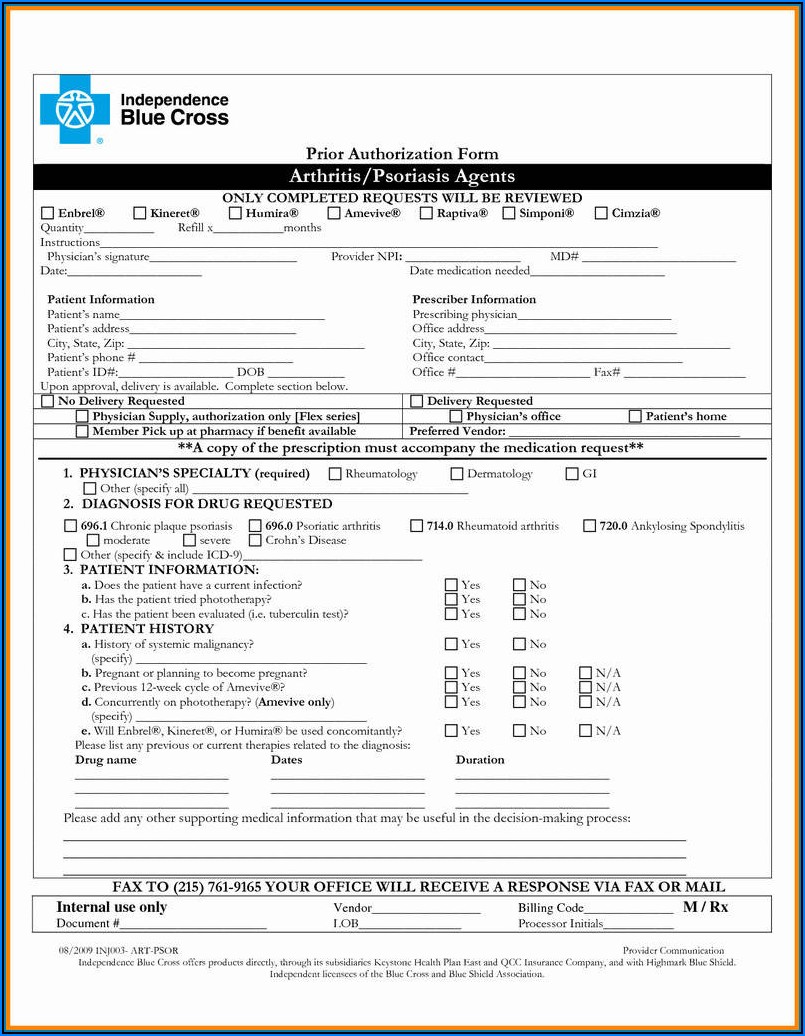
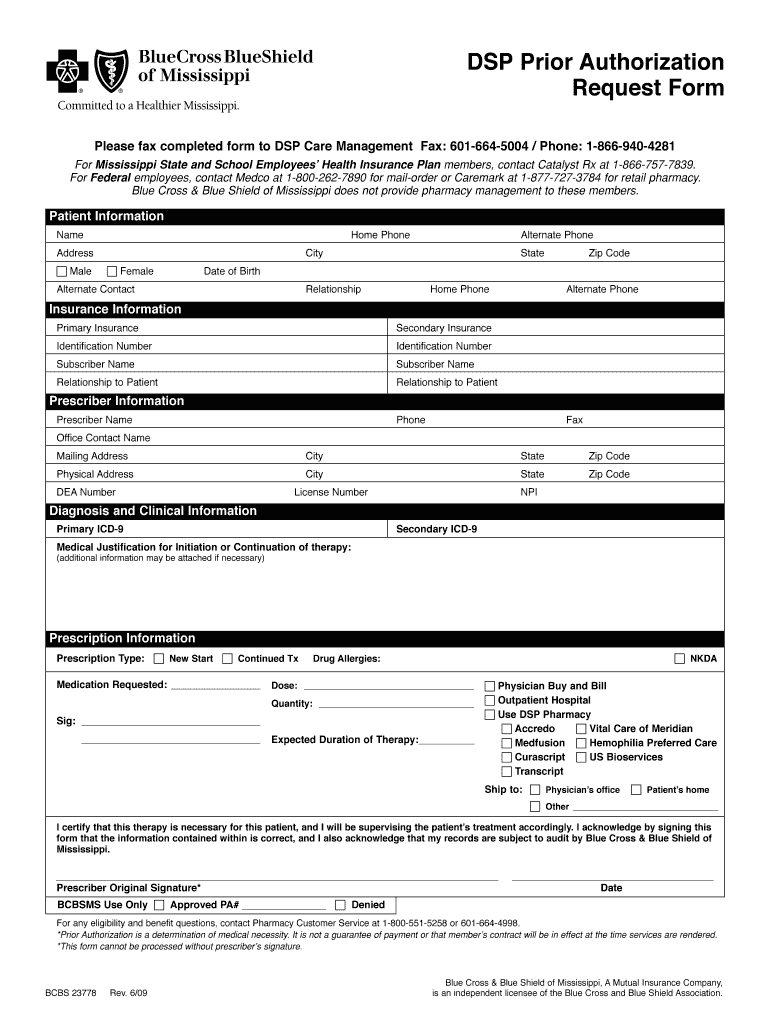
Blue Cross Blue Shield Of Mississippi Prior Authorization Form
Blue Cross Blue Shield Of Mississippi Prior Authorization Form - Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. If you are a network provider, use the myblue provider website to request a prior authorization. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the.
If you are a network provider, use the myblue provider website to request a prior authorization. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website.
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered.
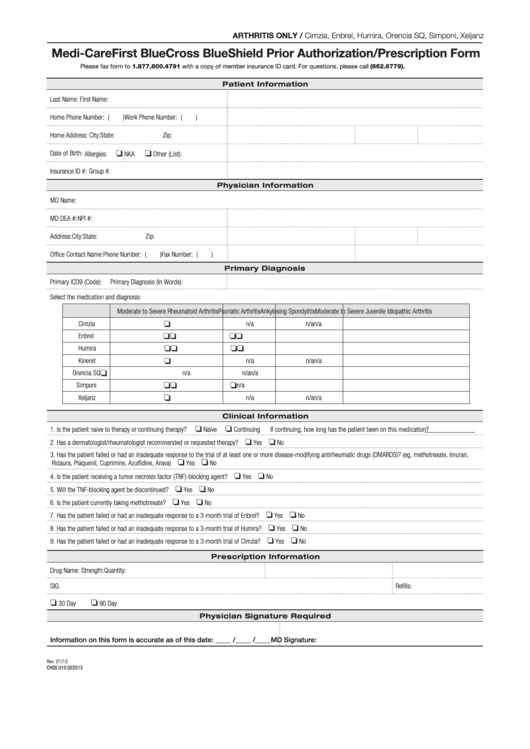
Fillable Online Blue cross blue shield medication prior authorization
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a network provider, use the myblue provider website to request a prior authorization. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If.
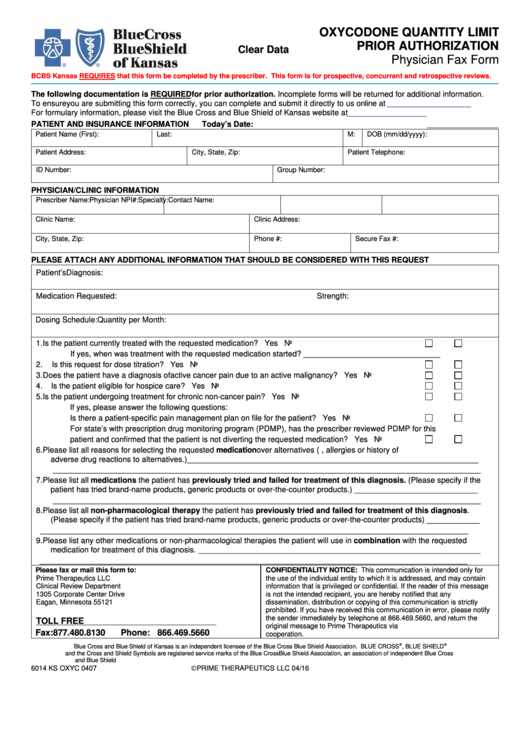
Blue Cross Massachusetts Prior Authorization Forms Form Resume
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If.
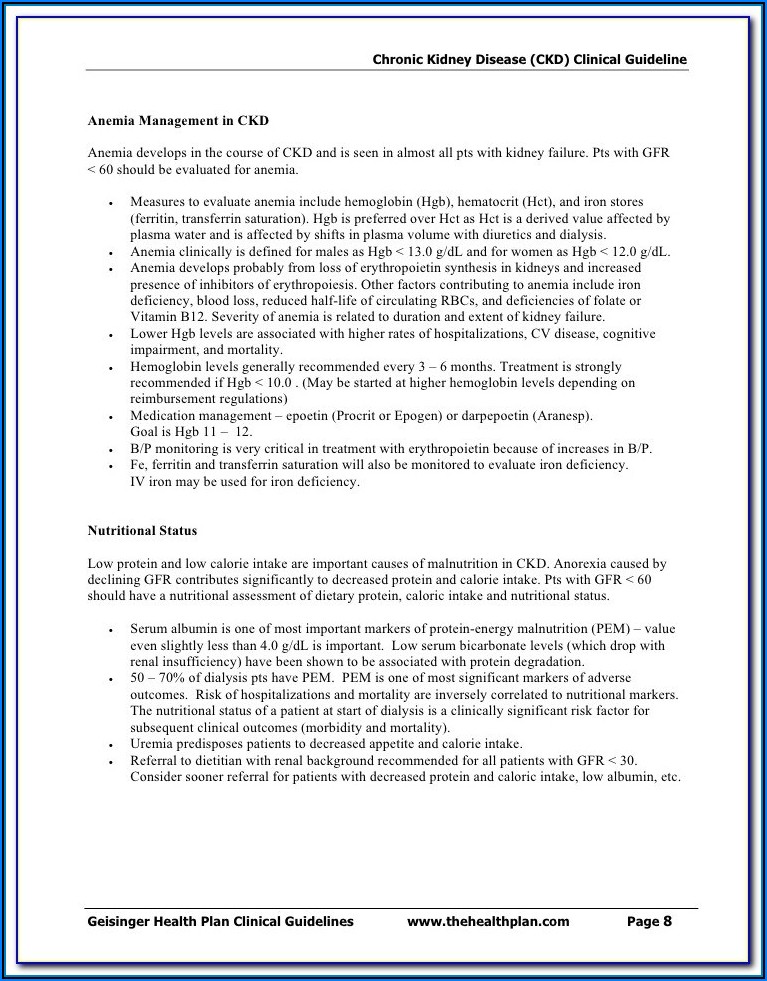
Fillable Medicare First Blue Cross Blue Shield Prior Authorization
If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. Certain drugs must be.
Blue Shield Highmark Bcbs Prior Auth Form
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription.
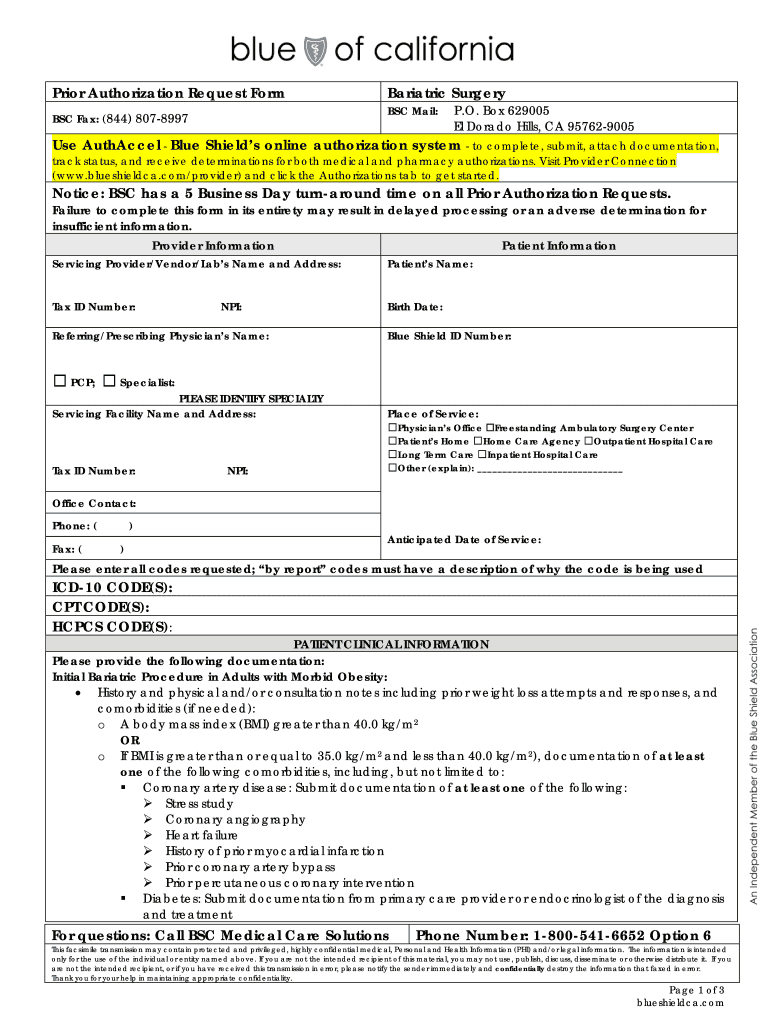
CA Blue Shield Prior Authorization Request Form Bariatric Surgery 2016
If you are a network provider, use the myblue provider website to request a prior authorization. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If.
Medicare Plus Blue Ppo Prior Authorization Form Form Resume
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a mississippi network provider, you should submit your prior authorization requests through our secure.
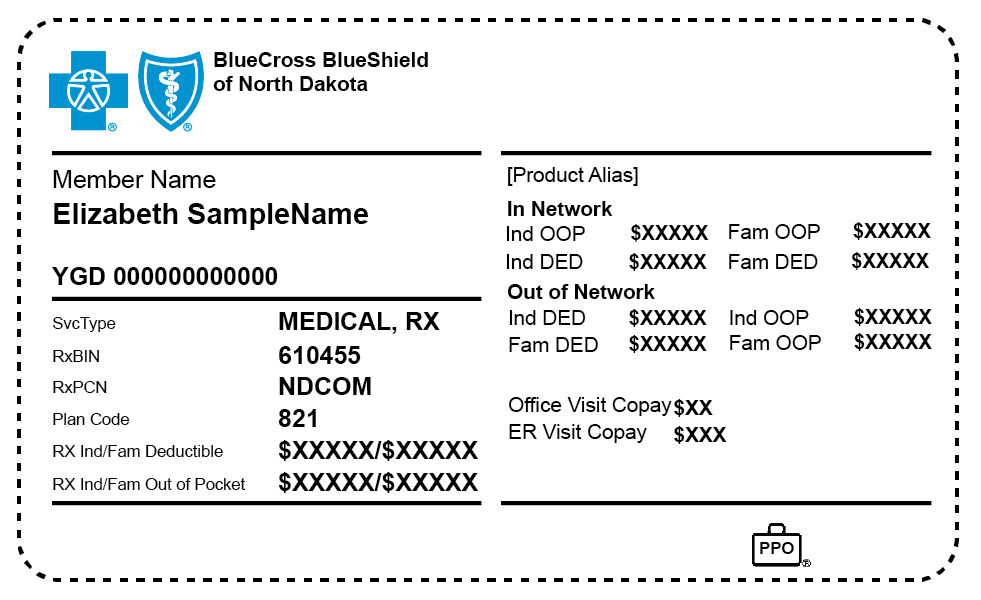
Authorized to Release Information BCBSND
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. If you are a network provider, use the myblue provider website to request a prior authorization. Prescription.
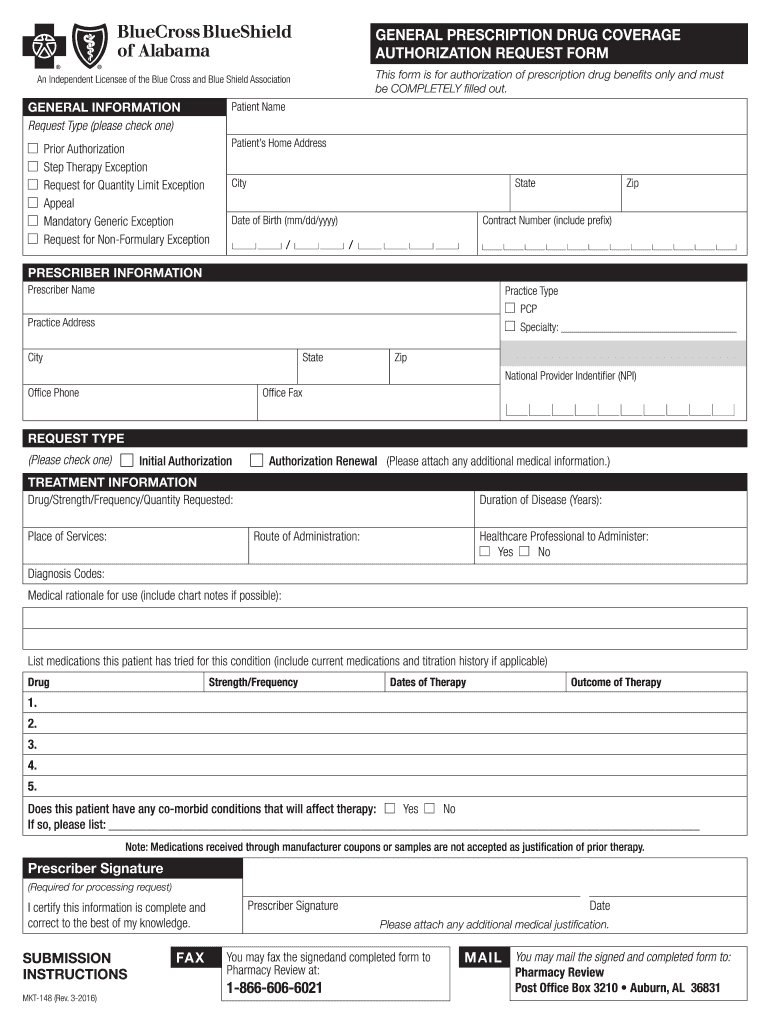
Blue Cross Blue Shield of Alabama Prior Authorization 20082024 Form
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. If you are a network provider, use the myblue provider website to request a prior authorization. Certain drugs must be.
Agreement reached between UMMC and Blue Cross Blue Shield of Mississippi
If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider.
Bcbs Of Mississippi Prior Authorization Form Fill Online, Printable
Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a network provider, use the myblue provider website to request a prior authorization. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website. Certain drugs must be.
If You Are A Network Provider, Use The Myblue Provider Website To Request A Prior Authorization.
Certain drugs must be prior authorized by blue cross & blue shield of mississippi, and dispensed by a network provider to be covered. Prescription drugs requiring a prior authorization are member/benefit plan specific and requires the member/patient’s name and id to start the. If you are a mississippi network provider, you should submit your prior authorization requests through our secure myblue provider website.